Dr. Robert Cerfolio says his "aha" moment came at the bedside of a COVID-19 patient, who seemed literally to be suffocating to death on his own mucus. After hearing the code for a cardiopulmonary arrest, Cerfolio had rushed into the unconscious patient's room and pulled out the thin ventilator tube delivering air into his lungs, to find it stopped up with discharge that had hardened to the consistency of concrete.
"Why aren't we doing a bronchoscopy?" Cerfolio called out, referring to a procedure where physicians snake a thin scope through the tube in a patient's airwaves and suck out obstructions. "This guy's not dying of COVID. He's dying of an obstructed tube!"
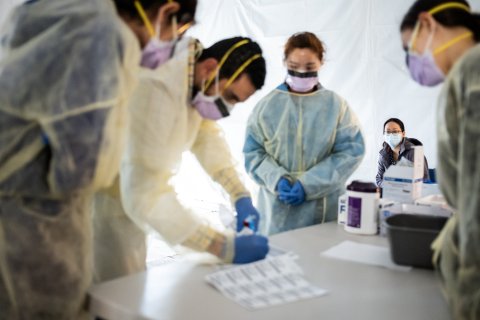
It was the early days of the crisis in New York City back when NYU Langone Health still had only a handful of COVID-19 patients. (The hospital declined Friday to give a precise current number, only saying "hundreds and hundreds.") The answer that came back from the doctors in attendance was not what Cerfolio expected to hear. We aren't allowed to, they told him. The procedure, which involved threading a smaller tube into the respirator conduit and down into the airways—and then pulling it out—could "aerosolize" the virus, dispersing it through the room and possibly infecting all the front-line health care workers around it. Which is why statements instructing against the procedure had been issued by a wide range of surgical and medical professional organizations.
Cerfolio, a thoracic surgeon whose many titles at the sprawling New York City medical center included senior vice president, vice dean and chief of hospital operations, was one of the few NYU Langone medical personnel in a position to override the directive. He was also the past president of the Thoracic Surgeons association, one of the organizations that had come out in opposition to the technique.
Cerfolio overrode the guidance. The patient lived. And Cerfolio and his colleagues at NYU Langone developed a new protocol for protective equipment and other precautions for doctors willing to do the procedure. They have since performed bronchoscopies on hundreds of COVID-19 patients.
Luis Angel, one of Cerfolio's colleagues, invented a new self-contained method for tracheostomies that can sometimes keep doctors from putting critically-ill patients on ventilators, which requires them to be put in a medically induced coma. The procedure, which requires incisions into the lower neck, is known to place health care providers at risk, but if safely performed allows doctors to use a bigger tube than is used for ventilation, one that is easier to clean.
NYU posted a video demonstrating the procedure, and Cerfolio's phone lines lit up.
"I've been called by the head of thoracic surgery at the main academic institution in Spain, I've talked to a guy in Italy and we're doing the exact opposite of what they have done there—even a friend at another hospital called me and said, 'I heard you guys are doing traches, what the hell you doing?'" Cerfolio says. "We've done 63 of these and not a single doctor or nurse has gotten sick—not one. Sixty-two of the patients are still alive. We know we can do it safely and we know we are helping patents."
As COVID-19 washes over the United States, doctors in hotspots across the nation are still deciding how best to battle a mysterious and deadly disease scientists don't yet fully understand. And while many are looking to the experience of health care providers in China and Europe, they are also racing to develop new procedures of their own and debating best approaches—often on the fly. In the fast-moving environment of a novel worldwide pandemic, there's not always time to wait for medical journals to publish. And the flood of reading material is growing so vast it's hard for many to track. So every day, clinicians around the world are helping each other as they find their way, trading and debating tips through social media, over conference calls and even over old medical school email chains.
On the other side of the nation, Dr. Tom Yadegar, a pulmonologist and medical director of the intensive care unit at Providence Cedars-Sinai Tarzana Medical Center in California, had his first "aha" moment when he got his first patients last month.
In those early days, he treated both a 60-year-old patient and an 80-something man, both of whom arrived stable, with good vitals, and normal X-rays, then spiraled into a rapid decline for seemingly no reason. Both ended up on ventilators, which drove Yadegar to the literature.
Through his research Yadegar realized that what he was seeing was a "cytokine storm," an overactive inflammatory reaction often seen in the sickest COVID-19 patients, a reaction so virulent it can kill. Soon he identified several blood markers, like the levels of ferritin, a protein that contains iron, that seemed to predict which patients were most likely to develop the overactive immune response. He wrote up protocols for his staff to follow that have them sometimes administering immunosuppressant drugs normally used to avoid organ rejection, to patients who seem likely to get in trouble.
"Up until a month ago, I didn't know about cytokine storms," he says. "I wasn't looking for it. It's not intuitive. And then to treat it, you're doing something that you probably have never done in your life, which is to give a patient in the ICU strong medications to suppress the immune system. It's totally counterintuitive."
Though similar protocols had previously been reported in China, Yadegar's experience was the first time many of his local peers had heard of the approach. He estimates he's kept three critically ill patients off of ventilators, and removed three more as a result of the protocol, and is now overseeing COVID-19 response in two affiliated area hospitals. Yadegar extended the impact of his finding by sharing his experiences with 50 or so fellow graduates of USC Medical School on a weekly call coordinated by his old program director. He then was interviewed about his approach on Fox and Friends, which prompted a flood of inquiries from other caregivers across the nation.
"This is such a new disease that all of us are struggling just trying to figure out what's going on," he says. "There's a lot of collaboration. We're all looking for answers."
Through these kinds of discussions and experimentation, unexpected observations are emerging that could transform care in the months ahead. One of the more significant is the debate about when best to place patients on ventilators.
Dr. Scott Weingart, a critical care physician at Stony Brook University Hospital, one of the busiest COVID-19 hospitals on Long Island, recently made an observation that he was literally able to broadcast out to the world. The key metric used to move patients to respirators is called "oxygen saturation," which measures how much oxygen is being held in a patient's blood. Usually, when a patient receiving oxygen through a normal mask can't get above 80 percent, doctors assume the lungs are compromised and the patient needs to be intubated. But Weingart was noticing that patients at levels that guidelines told him needed immediate ventilation weren't behaving like patients who were suffocating. Many, though short of breath, were able to speak in complete sentences, give full medical histories, and were even cheerful—a state he and his colleagues call "happy hypoxia."
Though Weingart couldn't explain the discrepancy, he began to suspect some unseen characteristic of the virus that scientists didn't yet understand was distorting the results. And he began second-guessing the protocols, waiting and watching.
"These levels are at numbers that would scare the hell out of us before this," he says. "But when we started holding off on putting those breathing tubes in and used simple measures like making the patient roll over in bed like you do every night while sleeping, all of a sudden there is a cohort, a group of these patients that didn't wind up needing the breathing tube."
Weingart, who hosts a popular podcast and blog followed by tens of thousands of ER doctors and critical care doctors, shared his experience on air and online—and heard from scores of others around the world who were noticing the same thing.
The finding is significant. Not just because it saves ventilators for sicker patients but because in order to go on a ventilator, the patient must be put in a medically induced coma, and there is anecdotal evidence that the pressure exerted by mechanical breathing machines can be injurious to the lungs of COVID-19 patients, Weingart says.
"Supportive care and watchful waiting have worked out in a lot of these COVID-19 patients, as opposed to what I call a knee-jerk response to sticking a tube down their throats," he says.
For physicians just now seeing their first patients—or still waiting for the full brunt of the pandemic to hit their areas—the experiences of frontline providers like Weingart, Yadegar and Cerfolio are proving invaluable. Sometimes the tips are as simple as telling conscious patients in the hallways to lie on their stomachs, instead of their backs, which results in more effective oxygen delivery to the portions of the lung involved in air-blood transfer. Some are learned through hard experience, such as that the use of the blood thinner heparin seems to help prevent potentially deadly blood clots in patients with BMIs greater than 40, who seem to be at greater risk of dying. (Both additional modifications recently adopted at NYU Langone). But the tips can also prove logistical.
In the weeks before she saw her first cases, Michelle Diaz, an ER physician who works at hospitals across New Hampshire through her company EMstaff, tuned in regularly to Weingart's podcast and others like it where she learned about the changing views on the timing of intubation. She also picked up numerous tips about what to expect and how best to prepare for it through an email chain that had previously been used to announce baby births by colleagues she had met while doing her residency back in the late aughts at Brooklyn's Kings County Hospital.
"One day somebody wrote that their hospital was still quiet and asked how everybody else was doing, and people just started posting stuff," Diaz recalls. "People are just sharing their experience, they are saying, 'I've seen this kind of clinical course, I tried this way of helping their oxygenation.' But also people are sharing ideas about what they're doing at their hospital to help with the volume and manage flow—'we have a tent set out over here and we have this personnel over there.'"
Diaz even learned how to she could convert a wall oxygen outlet into a BiPAP machine if she were to run out of equipment.
"These are things we thought we would never run out of—we never thought you would need to do this, but all of a sudden you might need to do this," she says. "And people are learning on the fly and things are changing fast. So it's been really helpful to see these ideas being exchanged. It's not just informative, it's inspiring."